On March 27, 2009, 89 active duty military trainees donated blood at a local blood center. Unfortunately, the trainees had received yellow fever vaccines (which contain live virus) only four days earlier. The Red Cross blood donation eligibility criteria requires a two-week wait after a yellow fever vaccine. The Red Cross does not test donated blood for yellow fever virus antibodies and the ineligible donations were not realized until the blood bank was preparing for another blood drive several weeks later. The contaminated blood was immediately recalled, tracked down and destroyed, but only after six units had been transfused into five patients.
One of the five patients who received a transfusion died, but as he was in hospice care for terminal cancer, it’s unclear whether the contaminated transfusion was responsible. Three of the four remaining patients had yellow fever antibodies in their system, but have not demonstrated any symptoms of yellow fever. The potential transmission of yellow fever to these patients is an impact to the patient safety goal. Additionally, the transfusion of contaminated blood impacts the compliance, organization, and patient services goals. The cost of the disposal of 83 contaminated units of blood is an impact to the materials goal, and the required investigation is an impact to the labor goal.
 The contaminated transfusions occurred because of the medical need for blood, and the use of contaminated donor blood. The donor blood was contaminated because the recall did not occur for several weeks (although it happened immediately after the contamination became known) and because the blood contained yellow fever antibodies. The yellow fever antibodies were present due to donors who had recently received vaccines, and donated, though ineligible. Because of the large number of trainees who donated blood despite being ineligible, it’s apparent that there was a disconnect in providing the information of a required two-week deferral from donation after vaccination.
The contaminated transfusions occurred because of the medical need for blood, and the use of contaminated donor blood. The donor blood was contaminated because the recall did not occur for several weeks (although it happened immediately after the contamination became known) and because the blood contained yellow fever antibodies. The yellow fever antibodies were present due to donors who had recently received vaccines, and donated, though ineligible. Because of the large number of trainees who donated blood despite being ineligible, it’s apparent that there was a disconnect in providing the information of a required two-week deferral from donation after vaccination.
Although the Red Cross does make its eligibility criteria known, it’s clear from this incident that this was insufficient in this case. The military has agreed to provide vaccination records for its members to ensure that blood is not donated during the deferral time after live virus vaccines. Additionally, the Red Cross has added specific, individual questioning about recent vaccinations. (The previous process used for screening with respect to recent vaccines was not discussed.) A recommendation is being made to have healthcare providers discuss eligibility for blood donation after vaccines are provided, though this is not currently being specifically required. These solutions should reduce the risk of providing contaminated blood.
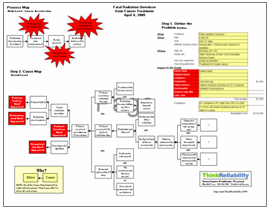
To view the one-page PDF containing the outline, Cause Map, timeline and action items, please click “Download PDF” above. The information for this investigation was provided by the Centers for Disease Control and Prevention (CDC)’s Morbidity and Mortality Weekly Report (MMWR).