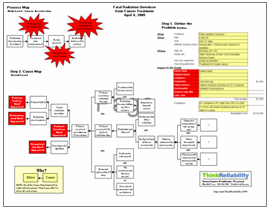
In October of 2005 a therapist was preparing a patient for radiation therapy. The therapist used a tattoo on the patient’s body to guide the radiation therapy. Additionally the therapist brought up a photo of the area to be irradiated. Unfortunately in this instance the tattoo and the photographs both indicated the patient’s esophagus – which was the site of previously delivered radiation therapy – instead of his upper spine, where the new radiation treatments were to be delivered.
 Although there was no damage to the patient’s health, this incident impacted the facility’s patient safety goal, because of the potential for injury to a patient when radiation is delivered unnecessarily. Additionally, it impacted the patient service goal because the radiation treatment was misdirected to the wrong body part. The organization and compliance goals were impacted because of this reportable error. Lastly, there are impact to the materials and labor goals due to the additional treatments that were required to deliver radiation to the upper spine.
Although there was no damage to the patient’s health, this incident impacted the facility’s patient safety goal, because of the potential for injury to a patient when radiation is delivered unnecessarily. Additionally, it impacted the patient service goal because the radiation treatment was misdirected to the wrong body part. The organization and compliance goals were impacted because of this reportable error. Lastly, there are impact to the materials and labor goals due to the additional treatments that were required to deliver radiation to the upper spine.
The situation was complicated by the software error that brought up an old picture, indicating that the therapy should treat the esophagus. To add to the confusion, there was a tattoo on the esophagus designating it as the site of the therapy. There was nothing in the set-up notes to indicate that the patient had had a previous round of radiation therapy. It is unclear whether the therapist had access to the patient’s chart, which would have designated the area to be irradiated and would mention the previous therapy.
The facility involved introduced measures to solve the software problems which resulted in the old photograph being downloaded. Second therapy sites are now marked with double tattoos. Information such as the therapy location and any previous radiation therapy sites are now included in the set-up notes. Additionally, ensuring that the therapist has access to a patient’s medical chart will help allow the therapist to ensure a patient’s therapy is delivered properly.
Step 3 to avoid radiation therapy errors: verify the WHERE – which body part requires the radiation therapy