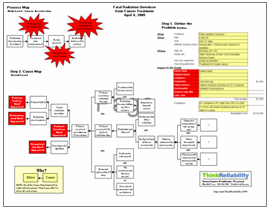
A cancer patient was scheduled to receive two radiation therapy treatments – radiation to her upper lung every day, and radiation to her mediastinum on alternating days. However, a mix-up resulted in her receiving the program for her lungs to her mediastinum (which resulted in ten times the prescribed dose) and receiving the program for her mediastinum to her lungs (which resulted in one-tenth the prescribed dose). The patient died of cancer later in the year.
This incident impacted the facility’s patient safety goal, because the patient died of cancer, possibly because the radiation dose to her lungs was too low to effectively fight the cancer. Additionally, it impacted the patient service goal because the patient received the wrong radiation treatment. The organization and compliance goals were also impacted because of this reportable error.
 How did this happen? The patient had a complex radiation therapy program, involving two different treatments to two different parts of her body simultaneously (radiation was delivered to different body parts on alternating days). Obviously some confusion on the part of the staff was involved, and because only one therapist was present for administering the therapy, there was no oversight, or anyone else to catch the error.
How did this happen? The patient had a complex radiation therapy program, involving two different treatments to two different parts of her body simultaneously (radiation was delivered to different body parts on alternating days). Obviously some confusion on the part of the staff was involved, and because only one therapist was present for administering the therapy, there was no oversight, or anyone else to catch the error.
Based on the causes of this incident, we can develop action items to be taken by the facility to reduce the risk of this type of incident happening again. Unless it is medically necessary, avoiding administering two different therapies at one time would reduce the risk of this type of confusion. The treatment a patient is receiving should always be verified before the treatment is administered. Also, because of the high level of risk to patients, more than one therapist should be present. (The facility involved in this particular incident has implemented a rule that more than one therapist be present for complex treatments. Although it’s not clear exactly what’s meant by complex, surely this would qualify.) Hopefully these steps, when taken by facilities who deliver radiation therapy to patients, will reduce the risk of radiation errors.
Step 2 to avoid radiation therapy errors: verify the WHAT – the type of treatment the patient is receiving.